Inflammatory Bowel Disease (IBD) is a chronic condition that affects the digestive system. It encompasses a group of disorders characterized by inflammation in the gastrointestinal tract, leading to various symptoms and potential complications. In this comprehensive guide, we will delve into the details of IBD, including its causes, types, symptoms, diagnosis, treatment options, and strategies for managing the condition.
1: What is Inflammatory Bowel Disease?
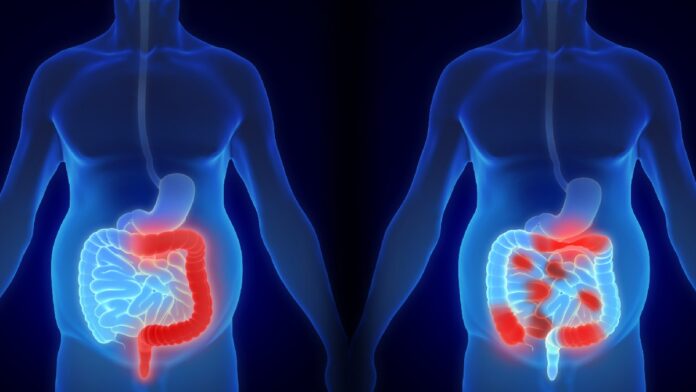
Inflammatory Bowel Disease, often abbreviated as IBD, refers to a group of chronic inflammatory conditions that primarily affect the gastrointestinal (GI) tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. These conditions are characterized by inflammation and can cause symptoms such as abdominal pain, diarrhea, and weight loss. IBD is different from irritable bowel syndrome (IBS), which is a functional GI disorder with different underlying causes and treatments.
2: Causes of Inflammatory Bowel Disease
The exact cause of IBD is not fully understood, but it is believed to result from a combination of genetic, environmental, and immune system factors. Some key points regarding the potential causes include:
1. Genetic Predisposition: People with a family history of IBD are at a higher risk, suggesting a genetic component.
2. Immune System Dysregulation: IBD is thought to develop when the immune system mistakenly attacks the healthy cells in the digestive tract, leading to inflammation.
3. Environmental Factors: Factors such as diet, smoking, and exposure to certain infections may contribute to the development of IBD.
4. Gut Microbiota: An imbalance in the gut microbiota (the community of microorganisms in the digestive tract) may also play a role in IBD.
5. Stress: While not a direct cause, stress can exacerbate IBD symptoms.
3: Types of Inflammatory Bowel Disease
There are two primary types of IBD:
1. Crohn’s Disease:
– Can affect any part of the digestive tract, from the mouth to the anus.
– Inflammation can be patchy and may extend through the entire thickness of the bowel wall.
– Can lead to complications such as strictures (narrowing of the intestine) and fistulas (abnormal connections between organs).
2. Ulcerative Colitis:
– Primarily affects the colon (large intestine) and rectum.
– Inflammation typically starts in the rectum and spreads continuously along the colon.
– Can lead to ulcers in the colon lining and may increase the risk of colon cancer.
4: Symptoms of Inflammatory Bowel Disease
Symptoms of IBD can vary in severity and may come and go. Common symptoms include:
1. Abdominal Pain: Crampy or constant pain in the abdomen.
2. Diarrhea: Frequent and urgent bowel movements, often with blood or mucus.
3. Weight Loss: Unintentional weight loss due to poor absorption of nutrients.
4. Fatigue: Ongoing tiredness and lack of energy.
5. Loss of Appetite: Reduced desire to eat.
6. Rectal Bleeding: Blood in stool, particularly in ulcerative colitis.
7. Joint Pain: Inflammation can affect joints, causing pain and swelling.
8. Skin Problems: Skin rashes and lesions may occur.
9. Fever: Occasional fever during flare-ups.
It’s important to note that IBD symptoms can overlap with other digestive conditions, so a proper diagnosis is essential.
5: Diagnosis of Inflammatory Bowel Disease
Diagnosing IBD involves a series of medical evaluations. The following are key diagnostic methods:
1. Medical History: A thorough discussion of symptoms, family history, and medical background.
2. Physical Examination: A physical examination of the abdomen and rectum.
3. Blood Tests: Blood tests can help identify signs of inflammation and nutritional deficiencies.
4. Stool Tests: Analysis of stool samples to check for blood, infection, and other abnormalities.
5. Imaging Studies: These may include X-rays, CT scans, MRI, or endoscopy (colonoscopy or sigmoidoscopy) to visualize the GI tract.
6. Biopsy: A tissue sample taken during endoscopy can confirm the presence of IBD and help differentiate between Crohn’s disease and ulcerative colitis.
6: Treatment of Inflammatory Bowel Disease
The management of IBD aims to control inflammation, alleviate symptoms, and improve the patient’s quality of life. Treatment options may include:
1. Medications:
– Anti-Inflammatory Drugs: Such as aminosalicylates, corticosteroids, and immunomodulators.
– Biologic Therapies: Targeted medications that suppress specific parts of the immune system.
– Anti-Diarrheal Drugs: To manage diarrhea.
– Pain Relievers: For abdominal pain management.
2. Nutritional Therapy: Special diets or nutritional supplements may be recommended to address malnutrition or inflammation.
3. Surgery:
– In severe cases or when complications arise, surgical removal of affected sections of the intestine may be necessary.
– In ulcerative colitis, removal of the entire colon (colectomy) may be required.
4. Lifestyle Modifications:
– Dietary changes: Avoiding trigger foods and adopting a well-balanced diet.
– Stress management: Techniques like meditation or counseling to reduce stress.
– Smoking cessation: If applicable, as smoking can worsen Crohn’s disease.
5. Supportive Care: Regular monitoring and support from a healthcare team, including gastroenterologists, nutritionists, and psychologists.
7: Coping with Inflammatory Bowel Disease
Living with IBD can be challenging, but there are strategies to help manage the condition:
1. Education: Understand your condition, treatment options, and potential complications.
2. Medication Adherence: Take prescribed medications as directed by your healthcare provider.
3. Dietary Management: Work with a dietitian to identify trigger foods and develop a suitable diet plan.
4. Stress Reduction: Practice stress-reduction techniques such as mindfulness, yoga, or deep breathing exercises.
5. Support System: Lean on friends, family, and support groups for emotional and practical support.
6. Regular Follow-Up: Maintain regular check-ups with your healthcare team to monitor your condition.
Inflammatory Bowel Disease is a complex, chronic condition that requires a comprehensive approach to diagnosis and treatment. While there is no cure for IBD, many individuals with the condition can lead fulfilling lives with proper management. If you suspect you have IBD or are struggling with symptoms, seek medical attention promptly. With the right guidance and support, individuals with IBD can effectively manage their condition and achieve an improved quality of life.
also read :
Understanding Breast Cancer: Causes, Symptoms, Diagnosis, Treatment, and Prevention